Published 11/1/19 by Anastasia Iliou
Medicare has certain rules and regulations in place to prevent fraud, waste, and abuse. Here’s one you may not have heard of – the 8-minute rule. Providers must treat patients for at least eight minutes to receive Medicare reimbursement.
What Is Medicare’s 8-Minute Rule?
Physical therapy billing guidelines for Medicare and Medicaid services include a section about how much time you must spend with a patient for it to be “bill-worthy.” Medicare physical therapy billing works in increments of 15. So what are you supposed to do when your treatment only takes 13 minutes to complete?
That’s where the eight-minute rule comes in. You only have to spend eight minutes with a patient to be able to bill for one “15-minute” unit. However, if you spend 16 minutes with a patient, you’ll still only be able to bill for one unit. You’d have to spend 23 minutes (15 + 8) with a patient to be able to fall into the two-unit bracket.

When The 8-Minute Rule Applies
The 8-minute rule only applies to time-based CPT codes for manual and physical therapy. This falls under Medicare Part B for outpatient therapy.
How Does the 8-Minute Rule Work?
The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes.
Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be standardized. You must complete at least eight minutes of treatment be paid for one 15-minutes increment.
So, for example, if you completed 17 minutes of treatment, Medicare would be billed for 15 minutes, or one unit. However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment. The bill would still be for two units regardless of whether you spent 23 or 30 minutes with the patient.
Guidelines for Medicare’s 8-Minute Rule
Billable units for the eight-minute rule would look something like this:
- 8 to 22 minutes of treatment = 1 unit
- 23 to 37 minutes of treatment = 2 units
- 38 to 52 minutes of treatment = 3 units
- 53 to 67 minutes of treatment = 4 units
- 68 to 82 minutes of treatment = 5 units
- Etc.
Mixed activities cannot be lumped together. What this means is that if you perform physical therapy with a patient for only five minutes, your timer resets before you begin the next activity. You cannot bill Medicare until you have worked with a patient on one activity for at least eight minutes.
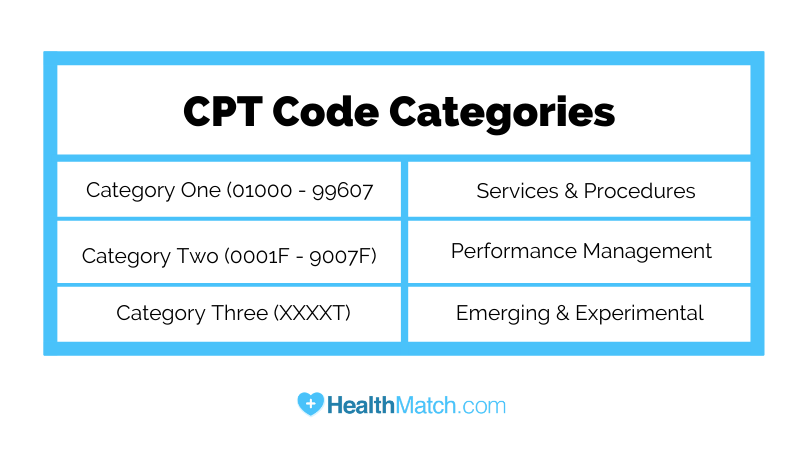
Current Procedural Terminology (CPT) Codes
As you may know, CPT codes are medical codes that describe the procedures and services you are performing to billing agencies and insurance companies. They were created by the American Medical Association in 1966 to simplify and standardize procedural reporting.
Each code consists of five characters. There are three code categories:
- Category 1 = services and procedures
- Category 2= performance management
- Category 3 = emerging and experimental services and procedures
Each category can be divided into sections. Category one contains:
- Evaluation and management services (numbers 99201 through 99499)
- Anesthesia (numbers 01000-01999)
- Surgery (numbers 10021-69990)
- Radiology (numbers 70010-79999)
- Pathology and labs (numbers 80047-89298)
- Medical services/procedures (numbers 90281-99607)
Category two contains:
- Composite measures (numbers 0001F-0015F)
- Patient management (numbers 0500F-0584F)
- Patient history (numbers 1000F-1505F)
- Physical exams (numbers 2000F-2060F)
- Diagnostics/screenings (numbers 3006F-3776F)
- Therapy/Preventive/Other interventions (numbers 4000F-4563F)
- Patient safety (numbers 6005F-6150F)
- Structural measures (numbers 7010F-7025F)
- Nonmeasure code listing (numbers 9001F-9007F)
Category three codes are temporary and will contain four numbers, followed by the letter “T.”
Physical therapy codes can be divided into service-based and time-based codes.
What are Service-Based CPT Codes?
Service-based CPT codes are as follows:
Physical Therapy Evaluations: 97161, 97162, 97163
Hot/cold packs: 97010
Unattended Electrical Stimulation: 97014
What Are Time-Based CPT Codes?
Time-based CPT codes are as follows:
Therapeutic Exercise: 97110
Therapeutic Activities: 97530
Manual Therapy: 97140
Neuromuscular Re-education: 97112
Gait Training: 97116
Ultrasound: 97035
Iontophoresis: 97033
Manual Electrical Stimulation: 97032
Time-Based vs. Service-Based CPT Codes
CPT Service-based billing is different from CPT time-based coding guidelines.
First of all, you’re probably wondering how the eight-minute rule works for minimal services, like applying cold compresses or completing a brief examination. Those services are not time-based, meaning regardless of whether it takes you 15 or 23 minutes to complete all of those minor items, you can only bill one unit.
You’ll need to use time-based units only for one-on-one, “constant attendance procedures.”
This is where billing gets tricky.
Let’s say you spend 25 minutes on a patient’s initial exam. During this time, you and your staff are asking and answering questions, taking a look at the affected area, etc. Then, let’s say you spend 20 minutes one-on-one with the patient performing a physical therapy exercise.
Technically, you’ve just spent 45 minutes with the patient, which would equate to three billing units. However, those first 25 minutes only counted for one unit because you were not in the room for the whole time, and you were not performing one undivided task. Therefore, you can only bill for two units.

Mixed Remainders
When you do the math for eight-minute rule billing, you might end up with a remainder that includes minutes from multiple services.
For example, let’s say you’ve performed 17 minutes of physical exercise and 21 minutes of manual therapy.
Individually, you’d only bill one unit for each of those, since you did not pass the eight minute threshold to put you into the next billing unit. However, you have two “remaining” minutes from the physical exercise and six “remaining” minutes from the manual therapy. Together, you have eight minutes, which would push you into the next billing unit.
Medicare guidelines would allow you to bill for three units in that circumstance.
8-Minute Rule Example
Alright, this has been a confusing lesson in billing! Let’s walk through an example putting everything we’ve learned together.
Mr. Jones, a patient with Original Medicare coverage, comes in for his scheduled appointment. You start with 20 minutes of examining Mr. Jones and asking him questions about his current state. You give him a cold pack for his injury while you’re talking. Then, you take eight minutes to perform an ultrasound. While you wait for those results, you set him up for 25 minutes of unattended electrical stimulation while you visit another patient.
Once the stimulation is done, you walk Mr. Jones through 20 minutes of manual therapy and 20 minutes of therapeutic exercise.
In total, Mr. Jones has been in the exam rooms for 93 minutes. 93 divided by 15-minute increments would equate to 6 billing units, but that’s not what is actually owed. Even though the electrical stimulation took 25 minutes, it was unattended. Therefore, it only qualifies for one billing unit.
Exam + cold pack = 20 minutes = 1 billing unit
Ultrasound = 8 minutes = 1 billing unit
Unattended electrical stimulation = 25 minutes = 1 billing unit
Manual therapy = 20 minutes = 1 billing unit
Therapeutic exercise = 20 minutes = 1 billing unit
Your billing department would send Medicare a bill for five billing units for Mr. Jones.
Does The 8-minute Rule Apply to All Insurances?
No! Not necessarily. By definition, the 8-minute rule applies to Medicare, Medicaid, TRICARE, and CHAMPUS. Private insurance carriers may choose to operate the same way, but by rule are not required to. Medicare beneficiaries who enroll in private Medicare plans (Medicare Advantage) may also have different billing standards depending on the plan.
AMA 8-Minute Rule & The Rule of Eights
You’ll find the “rule of eights,” sometimes called the AMA 8-Minute Rule, within the CPT code manual. This CPT rule is slightly different from the CMS rule for Medicare and Medicaid.
The general concept is the same – billing occurs in 15-minute increments, with over eight minutes of service counting for one 15-minute increment. However, time is not combined. Each 15-minute increment of service is treated as if it is billed separately. There are no mixed remainders.
This AMA timed code means that if you perform one physical therapy service for 16 minutes, and another for 22, you’d only bill for two units, instead of combining the extra one minute from the 16-minute service and the extra seven minutes from the 22-minute service to create a third unit.
Other insurers might use AMA timed codes instead of CMS timed codes.
The Best Way to Avoid 8-Minute Rule Mistakes
Considering that it took us over 1,000 words to explain this one billing process, it can be pretty easy to perform incorrectly. We definitely recommend NOT trying to do the math yourself for every patient.
Billing programs (like WebPT, who we’ve cited a few times in this post) offer calculators that will do all this for you. As long as you have the patient’s insurance information correct and you have someone correctly entering all of your electronic health records correctly, you can’t mess up the eight-minute rule.
Who is HealthMatch.com?
HealthMatch.com is a third-party communication center for doctors and other medical professionals.
We can help your patients schedule their annual wellness visits, change their insurance, whatever your practice needs!
To get in touch with a HealthMatch.com implementation manager, call 1-844-551-1755 or send us a text here.
Anastasia is the Senior Content Manager for HealthMatch.com. After majoring in Songwriting at Belmont University, Anastasia discovered a passion for long-form written content. In her spare time, she enjoys spoiling her two cats and two dogs.